Prostate-Specific Antigen (PSA) Test
The PSA blood test is used to help diagnose prostate cancer. The test is a valuable and potentially life-saving screening test for many men, as well as transgender women. Prostate cancer kills more men than any other cancer except lung cancer.
However, the PSA test is an imperfect test. It cannot reliably tell the difference between slow-growing prostate cancers that do not pose any serious health risks and fast-growing cancers that are less common but more deadly. Men with low-risk cancers may then be subjected to unnecessary tests, such as prostate biopsies. They may also undergo unnecessary treatments (for example, surgery, radiation therapy) that may cause upsetting side effects, such as erectile dysfunction and urinary incontinence.
In general, all cancer screenings are beneficial. But when the risks associated with testing outweigh the potential benefits, the test may actually do more harm than good. For this reason, the PSA test is typically only recommended for men at high risk for prostate cancer due to their age or other risk factors.
How can you know whether you should get a PSA test or not? Screening for prostate cancer is an individual decision that a man should make with his doctor’s help based on factors such as his level of risk, overall health, life expectancy and willingness to undergo treatment in the event of a prostate cancer diagnosis.
Learn more about PSA testing in the following Q&A:
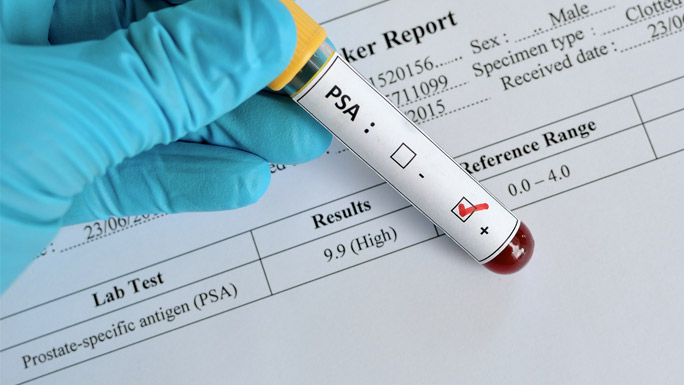
As the name suggests, the PSA test measures the amount of a substance called prostate-specific antigen (PSA) in your blood. The prostate, which is a small reproductive gland near the bladder, continually makes PSA on a regular basis. Typically, men have low levels of PSA in their blood. But when PSA levels are high, it could be a sign of cancer or other problems, such as an infection or an enlarged prostate.
At UChicago Medicine, urologists and other physicians follow the prostate cancer screening guidelines from the American Urology Association and the American Cancer Society.
These guidelines recommend that every man talk to his physician about whether/when he needs a PSA test. Your doctor can help you identify your risk for prostate cancer, explain the benefits and potential harms of the test, and help you decide whether/when to get the test given your personal values and circumstances.
As discussed above, the PSA test is very good at identifying prostate cancer. However, it cannot discern between aggressive cancers that need immediate treatment and slow-growing, low-risk cancers. It also cannot discern between cancer and other conditions that elevate PSA levels in the blood, such as an enlarged prostate.
Thus, PSA tests provide the most value to men of certain ages and with certain risk factors.
For men under age 55: Younger men do not usually need to get PSA tests. Prostate cancer is rare in younger men.
But you and your doctor may decide that you could benefit from getting the test if you have a higher than average risk for developing prostate cancer. Risk factors linked to prostate cancer include:
- Having one or more relatives who has or had prostate cancer, including father, brothers, uncles or grandfathers
- Being of African descent
- Being of Ashkenazi Jewish ancestry
- Carrying certain cancer-related genetic mutations, such as BRCA 1, BRCA 2, ATM, and CHEK2, found to increase the risk of prostate cancer
- Having a family history of any type of aggressive adenocarcinoma cancer (which start in the glands of organs)
- Adenocarcinomas include prostate, breast, ovarian and pancreatic cancers.
UChicago Medicine has a special program, called the High Risk & Advanced Prostate Cancer Clinic, that provides a comprehensive genetic evaluation to determine your risk of prostate cancer. If you are found to have an elevated risk, we will put together a multifaceted plan that spells out the screening tests you should get and how often.
For men ages 55 to 69: The greatest benefit of screening for prostate cancer appears to be in men of this age. Prostate cancer is most likely to occur at this time of life.
For men ages 70 and older: Research shows that men with a life expectancy less than 10 to 15 years will not likely benefit from aggressive treatment for any prostate cancer discovered by the PSA test. That’s because most prostate cancers discovered at this age are slow growing.
However, men ages 70 and older who are in excellent health and can expect to live longer than 10 years may benefit from regular PSA tests. They should talk to their doctor about the benefits and risks.
However, men who had high PSA levels on their first or last PSA test may benefit from more frequent screenings. Your doctor can help you determine when exactly you need to get another test.
As the prostate cancer advances to the intermediate stage, men may experience urinary issues, such as pain or burning when urinating, a weak flow of urine, or the need to urinate frequently. However, other non-cancerous health problems, such an enlarged prostate, can also cause urinary issues.
When prostate cancer is advanced, men may have symptoms in addition to urinary problems, such as blood in the urine and loss of appetite.
You should postpone getting a PSA test:
- When you are actively ill
- When you are intoxicated
- If you have a prostate infection or inflammation
- If you have an indwelling Foley catheter
- If you have recently engaged in strenuous physical exercise or activities (for example, riding a bike, rowing)
In all these circumstances, you are more likely to have a false-positive PSA test, or high levels of PSA in your blood that is not related to prostate cancer.
Typically, the urologist will perform a digital rectal examination (DRE) to feel for any abnormalities of prostate and order a repeat PSA. If the repeat PSA test shows elevated PSA levels, your urologist may recommend additional tests to determine whether you may have prostate cancer or another problem like an enlarged prostate.
In the past, most men with high PSA levels would have to undergo a biopsy, which involves inserting a thin needle through the rectum to remove a small sample of the prostate gland to test for cancer. But, today, not every man with suspected prostate cancer needs a biopsy, which can cause soreness, bleeding and other unpleasant side effects.
Recent advances in laboratory testing and imaging studies have made it easier for physicians at UChicago Medicine to make an accurate diagnosis without a biopsy. A number of novel blood and urine tests can be used to reliably discern whether a patient has an aggressive prostate cancer. Our pathologists are nationally known for their expertise in pinpointing cancer subtypes.
In addition, we have a range of advanced imaging tests, including a state-of-the-art prostate MRI and PSMA PET, that provide the best available pictures of the prostate and any potential prostate cancers.
In some cases, laboratory and imaging tests will indicate the need for a biopsy. Our physicians are experts in targeted, minimally invasive approaches to prostate biopsy, reducing potential side effects.
Learn more about the state-of-the-art prostate cancer tests available at UChicago Medicine, as well as treatment for prostate cancer.
Request an Appointment for a PSA Test
UChicago Medicine offers PSA tests at several locations in Chicago and the surrounding suburbs. Request an appointment with a primary care physician to discuss if PSA testing is right for you by:
- Scheduling a primary care appointment online (select internal medicine or family medicine)
- Calling 1-888-824-0200 to speak with a referral counselor who can schedule your appointment
- Searching for a primary care physician near you
- Finding a primary care location near you

Cancer Care Second Opinions
Request a second opinion with a UChicago Medicine urologic cancer expert.

High Risk & Advanced Prostate Cancer Clinic
Focused care for men at risk for prostate cancer and those with advanced disease.

Participate in a Prostate Cancer Clinical Trial
UChicago Medicine physician-scientists are actively conducting clinical trials of new therapies for prostate cancer.
